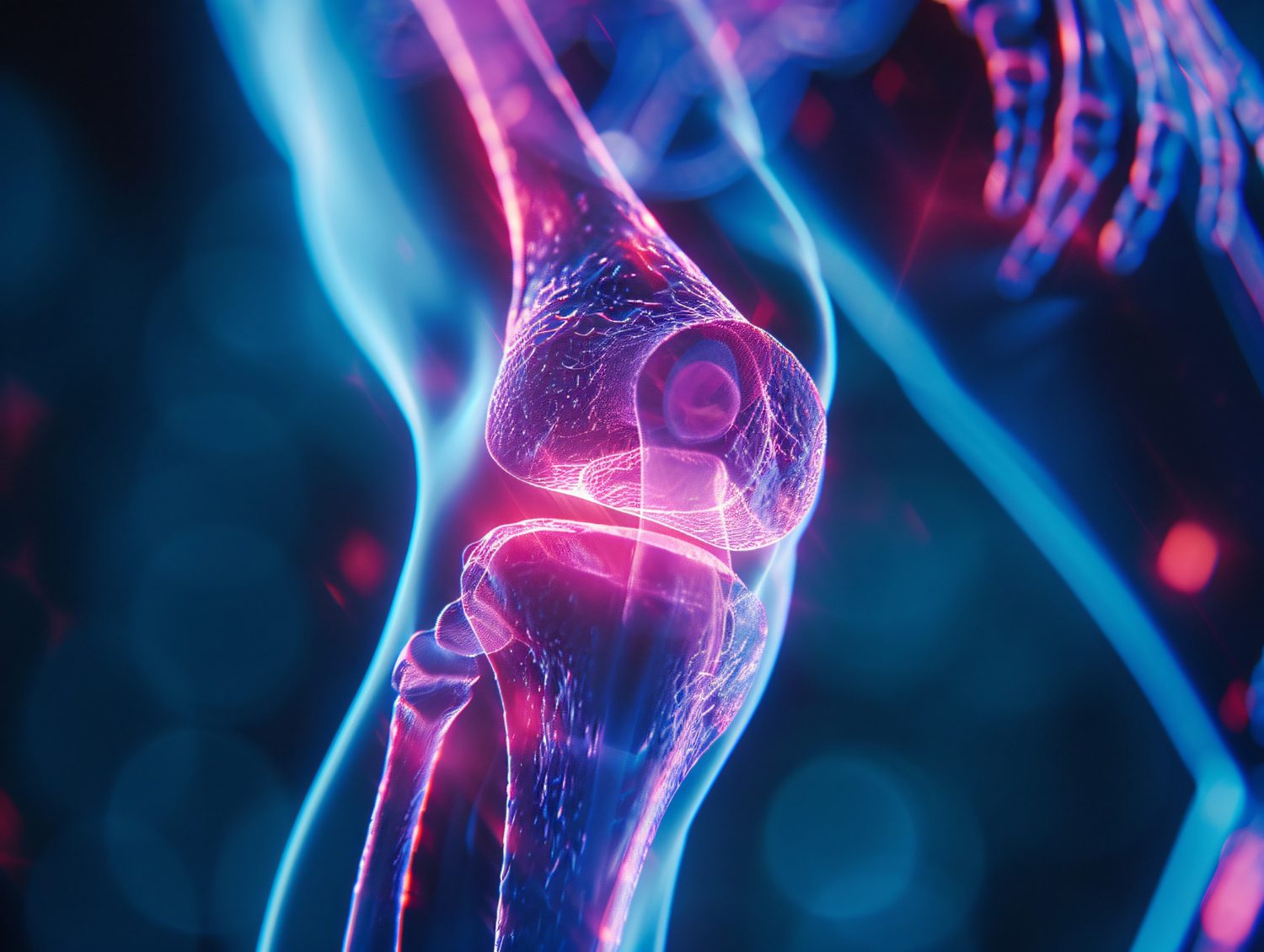
It refers to a pathological condition characterized by the irritation and swelling of the synovial membrane – a specialized connective tissue encasing joint cavities. This condition frequently induces discomfort, joint immobility, and swelling, impairing routine activities. Though commonly linked with knee synovitis, it can also impact the hip, shoulder, elbow, ankle, or wrist, making it a pervasive yet frequently overlooked issue that necessitates meticulous evaluation and customized therapeutic strategies.
These ailments provoke localized edema, articular immobility, and discomfort, impeding daily motions. Hip synovitis often hinders walking or weight-bearing, while shoulder synovitis restricts rotational capacity. Elbow synovitis impairs lifting actions, and ankle synovitis disrupts stability, complicating ambulation. Wrist synovitis, commonly overlooked, restricts dexterity and fine motor tasks.
Mitigation demands prompt detection and tailored intervention, involving non-invasive regimens like cryotherapy, pharmacological solutions like corticosteroid-injections, or surgical measures for severe afflictions. Regular low-impact exercise and ergonomic adjustments safeguard against recurrence, ensuring joint vitality.
Synovitis Symptoms: Detecting Early Signs
Accurate recognition of synovitis symptoms enables prompt intervention, averting complications and long-term deterioration. Key manifestations encompass next-described.
- Localized Edema: Visible puffiness enveloping the afflicted joint, often accompanied by tenderness.
- Articular Rigidity: Impaired ability to perform rudimentary motions such as flexing, rotating, or lifting extremities.
- Painful Sensations: Throbbing, piercing, or dull discomfort exacerbated by movement or external pressure.
- Thermal Fluctuations and Erythema: Affected zones may feel unusually warm and display a reddish discoloration.
- Crepitation: Audible grinding or cracking noises during movement, indicating structural irritation.
Identifying these hallmark indicators facilitates timely synovitis diagnosis, enhancing prospects for effective mitigation.
Synovitis Causes: Identifying Underlying Factors
Comprehending synovitis causes is paramount for devising preventative measures and sustainable remedies. Potential triggers include next-described.
- Traumatic Synovitis: Attributed to acute injuries such as strains, contusions, or direct impacts.
- Inflammatory Synovitis: Deriving from persistent conditions such as gout or rheumatoid ailments.
- Infectious Synovitis: Initiated by microbial agents infiltrating the synovial layer.
- Autoimmune Synovitis: Occurs when the immune apparatus erroneously targets synovial structures.
- Reactive Synovitis: Secondary to systemic maladies or distant infections.
Addressing these contributory factors minimizes recurrence and bolsters outcomes.
Synovitis vs. Arthritis: Clarifying the Distinctions
Often conflated, synovitis and arthritis differ fundamentally. Synovitis involves isolated irritation of the synovial lining, whereas arthritis encompasses joint inflammation, cartilage erosion, and potential osseous damage. Precise differentiation ensures accurate synovitis diagnosis and optimized therapeutic selection.
Synovitis Treatment: Effective Modalities
Effective synovitis treatment integrates both conservative and invasive approaches, depending on severity and underlying causes. Common modalities include next-described. Leave a request for a consultation with a specialist who will help you choose an effective treatment.
Non-Invasive Interventions
- Rest and Joint Safeguarding: Restricting joint movement to alleviate strain on the compromised area.
- Cryotherapy and Thermotherapy: Alternating cold packs with heat applications to soothe discomfort and reduce rigidity.
- Compression and Elevation: Utilizing bandages or supports to stabilize joints and mitigate fluid buildup.
Pharmacological Remedies
- Synovitis Medication: NSAIDs (non-steroidal anti-inflammatory drugs) to alleviate pain and counteract swelling.
- Corticosteroids: Administered via injections for immediate relief in acute cases or persistent chronic synovitis.
- Disease-Modifying Agents: Prescribed for autoimmune-linked synovitis to control overarching systemic afflictions.
Synovitis Surgery
- Synovectomy: Extraction of inflamed synovial tissue for refractory knee synovitis or other joints.
- Joint Debridement: Cleansing joint spaces to rectify functional impairments and avert degeneration.
Add a separate statement for stem cell therapy, calling it the most advanced, and it is something between surgery and a pharmacological approach.
Acute vs. Chronic Synovitis: Key Differentiators
- Acute Synovitis: Develops abruptly, frequently following trauma or infection, presenting with rapid-onset swelling and intense discomfort.
- Chronic Synovitis: Progresses gradually, often due to underlying autoimmune conditions, resulting in enduring joint distress and deformities.
Tailored intervention is vital for addressing the nuances of both types.
Preventive Measures for Synovitis
Adopting preemptive measures diminishes the likelihood of developing or exacerbating synovitis. Strategies include next-described.
- Ergonomic Adjustments: Optimizing posture and joint alignment during repetitive tasks.
- Regular Activity: Reinforcing musculature surrounding joints to augment resilience and mobility.
- Protective Apparatus: Employing braces or pads to absorb impacts, especially in traumatic synovitis prevention.
- Nutritional Support: Incorporating omega-3-rich foods and antioxidants to mitigate systemic inflammation.
Synovitis Recovery: Anticipating Outcomes
Recovery durations vary based on the condition’s severity and selected interventions. Minor cases may resolve within weeks, while chronic synovitis might necessitate surgical measures, specialized therapies, or sustained lifestyle modifications.
Synovitis Exercises: Promoting Joint Resilience
Targeted regimens ensure enhanced mobility and diminished recurrence. Recommendations include next-described.
- Gentle Stretching: Controlled elongation and flexion of limbs to preserve flexibility.
- Isometric Exercises: Gradual muscle activation sans joint strain to restore strength.
- Low-Impact Activities: Swimming or cycling to alleviate stress on vulnerable joints.
Leave a request for a consultation with a specialist who will help you choose the right treatment and monitor the progress of your recovery.
What is synovitis?
Synovitis signifies inflammation of the synovial tissue lining joint cavities. It leads to swelling, stiffness, and discomfort, frequently necessitating diagnostic scrutiny.
How is synovitis treated?
Treatment encompasses rest, synovitis medication, physical therapy, and surgical techniques for severe instances. Proper strategies ensure optimal recovery.
What causes synovitis?
Triggers include trauma, autoimmune conditions, microbial infections, and repetitive stress. Underlying illnesses may also cause reactive or inflammatory synovitis.
Can synovitis be cured?
In most instances, synovitis can be managed effectively with early intervention and appropriate therapies. Chronic synovitis, however, may require continuous monitoring and lifestyle adjustments to control relapses. Consultation with a heal-thcare expert is highly-recommended. Their expertise guarantees an accurate diagnosis and personalized treatment solutions.