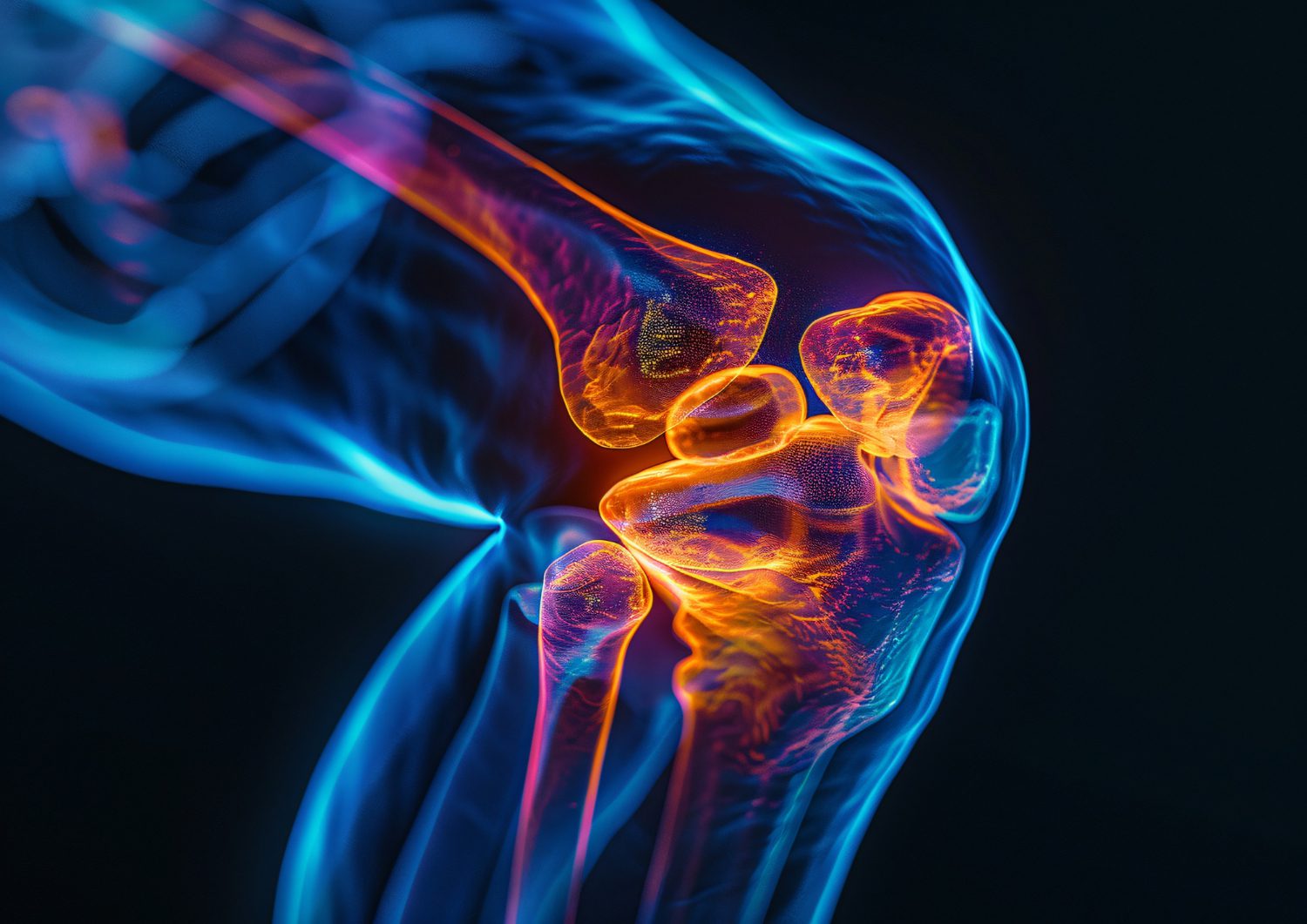
Osteoarthritis is a degenerative joint disease DJD characterized by the gradual breakdown of protective cartilage, leading to joint pain, stiffness, and reduced mobility .It progressively deteriorates protective cartilage, impairing articulation, inducing persistent discomfort, and limiting flexibility. Unlike inflammatory arthritis, osteoarthritis disease predominantly stems from cumulative wear-and-tear, establishing its distinction from auto-immune disorders like rheumatoid arthritis. This ailment influences diverse joints, manifesting variably as knee and hip osteoarthritis, or even osteoarthritis in hands.
Root Triggers of Osteoarthritis and Arthritis
Degenerative osteoarthritis emerges from interconnected genetic, mechanical, and environmental influences. Principal osteoarthritis causes include next-described.
- Age-Driven Cartilage Attrition: Natural cartilage degradation accelerates post-middle-age.
- Repetitive Joint Trauma: Fractures or ligament injuries can provoke degenerative changes.
- Obesity-Related Joint Strain: Excessive body-weight increases stress-reactions, particularly on load-bearing joints.
- Hereditary Susceptibility: Familial patterns often indicate genetic predispositions.
- Skeletal Misalignment: Abnormal joint structures foster cartilage erosion.
Recognizing its symptomatic features early aids proactive interventions. Common manifestations involve stiffness, audible clicks, and intumescence, which progressively worsen without attention.
Symptoms and Manifestations of Osteoarthritis
Accurate identification of osteoarthritis symptoms is paramount for timely management. Frequently reported indicators comprise next-described.
- Persistent Joint Ache: Pain intensifies during movement or exertion.
- Restricted Motion Range: Joint rigidity hampers normal mobility.
- Recurring Swelling: Inflammation heightens discomfort and reduces agility.
- Cracking Sensations: Audible joint noises sometimes accompany flexion or movements.
Influenced areas range from knee osteoarthritis to spondylosis osteoarthritis, underlining its diverse effect on human physiology.
Strategies for Degenerative Joint Disease Treatment
Managing degenerative joint disease requires integrative approaches, prioritizing personalized care. Effective degenerative joint disease treatment involves next-described.
- Lifestyle Interventions: Nutritional optimization, including an osteoarthritis diet rich in omega-3s, antioxidants, and anti-inflammatory components (e.g., turmeric, green tea).
- Low-Impact Routines: Gentle exercises for osteoarthritis, like swimming, tai chi, or yoga, encourage mobility while reducing joint strain.
- Assistive Solutions: Orthotic devices or compression gear alleviate pressure during activities.
- Osteoarthritis Medications: Non-steroidal anti-inflammatory drugs (NSAIDs), topical analgesics, or corticosteroid injections mitigate inflammation and uncomfortable feelings.
- Advanced Therapeutics: Surgical interventions – joint replacements – are reserved for highly-serious or unresponsive states.
Leave a request for an appointment with a specialist who will help correctly assess the disease and provide recommendations for further actions.
Preventing Osteoarthritis: Lifestyle Adjustments
Effective prevention integrates sustainable habits aimed at minimizing risk factors. Key recommendations for preventing osteoarthritis include next-described.
- Weight Control: Maintaining appropriate body weight reduces undue joint stress.
- Postural Awareness: Proper alignment during daily activities guards against premature cartilage wear.
- Regular Movement: Controlled mobility, through stretching or low-intensity exercises, enhances flexibility and supports joint health.
- Avoiding Repeated Strain: Minimizing repetitive actions that intensify cartilage breakdown.
Struggle Methods and Diagnostics
Osteoarthritis pain relief methods incorporate targeted techniques like heat/cold therapy, acupuncture, or physiotherapy. For accurate osteoarthritis diagnosis, healthcare practitioners employ X-rays, MRI imaging, or joint fluid analysis, ensuring precise assessments.
Osteoarthritis vs. Rheumatoid Arthritis: Key Differences
While both arthritis and osteoarthritis affect joint structures, their origins diverge significantly. Osteoarthritis stems from cartilage erosion, whereas rheumatoid one arises from immune-mediated synovial inflammation. Fully-realising their differences supports accurate diagnoses and tailored care strategies.
What is osteoarthritis?
Such ailment, degenerative joint sickness, results from cartilage erosion, leading to stiffness and impaired mobility. Unlike inflammatory conditions, it primarily arises from long-term mechanical wear.
How does osteoarthritis make you feel?
It triggers chronic aches, joint stiffness, and restricted movement. After some time, it may lead to swelling or grating sensations during articulation.
Is osteoarthritis manageable?
Yes, osteoarthritis is manageable through early diagnosis, proper interventions, and consistent care. Adjusting lifestyle routines, using appropriate osteoarthritis medications, and engaging in physical therapies significantly diminish its symptomatology.
What is the best osteoarthritis treatment?
Optimal osteoarthritis treatment combines dietary adjustments, therapeutic exercises, and targeted medical care. In highly-serious states, surgical therapies – joint replacement – provide long-term relief. A consultation with a qualified healthcare provider is crucial. They will help confirm the presence of osteoarthritis and guide you through the required management strategies.